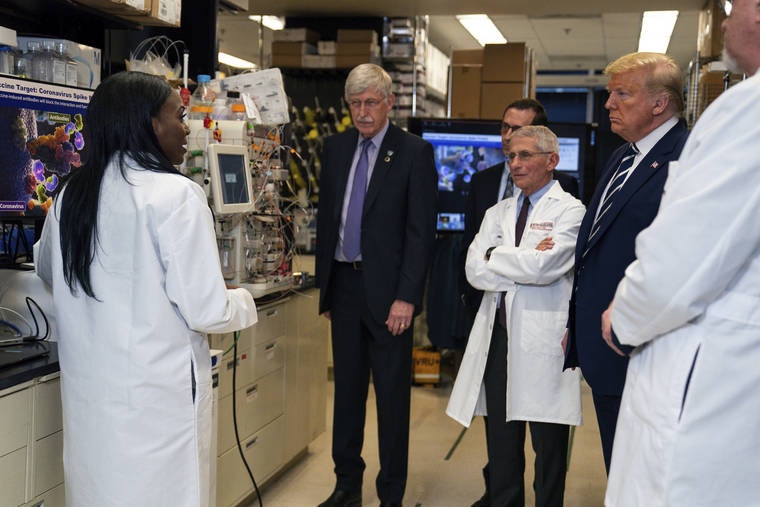
Dr. Kizzmekia Corbett, pictured left, Senior Research Fellow and Scientific Lead for Coronavirus Vaccines and Immunopathogenesis Team in the Viral Pathogenesis Laboratory, talked with President Donald Trump, March 3, as he toured the Viral Pathogenesis Laboratory at the National Institutes of Health in Bethesda, Maryland, U.S.
1. Can you tell us more about yourself and your educational background?
This is always an interesting question for me to answer. I’m a viral immunologist, by training. In fact my science training started in high school when I spent a couple of summers working in a chemistry lab at UNC, funded by a program called “Project SEED”. Then I went to UMBC where I was a Meyerhof scholar and double Biology and Sociology major. During that time, I was also a NIH UGSP scholar and thus trained at NIH during the summers. After undergrad, I went to UNC and obtained my PhD in microbiology and immunology.
2. What influenced you to pursue a phD in the field of microbiology and immunology?
Having trained at the VRC during undergrad, I gained a passion for vaccine development, specifically for viruses that evade vaccine responses. So it was a clear path in that way. Understanding fundamental human immune responses is key to informing vaccine development.
3. You are at the frontline of developing a potentially revolutionary vaccine for the 2019- nCoV virus. What are some of the main challenges that you face when developing a vaccine?
Too little time. *laughs* I say that jokingly but also in truth. We were able to implore a clinical trial in 66 days after sequence release of SARS-CoV-2, and literally since Jan. 10th… our work has been nonstop. I plan to be this busy for the next year at least because there are fundamental experiments to be completed to move our vaccine further into clinical trial phases and hopefully into the general population.
4. Interestingly, the vaccine you are currently testing in phase 1 clinical trials uses mRNA technology. Could you give a brief explanation of how this works?
Messenger RNA essentially tells cells what to do. In our case, we are using a SARS-CoV-2 spike protein that we designed with collaborators at UT Austin. Using Moderna’s mRNA platform we are able to tell cells to make the spike protein that would then trigger the immune response to later protect one from infection. This is a plausible strategy because the spike protein is used by the virus to attach to cells. By targeting immune responses to spikes, we can effectively block infection.
5. You’ve worked extensively on Dengue virus and Middle East Respiratory Syndrome Coronavirus. Were there any lessons from those scientific endeavours that inform you when researching 2019-nCoV?
You know, I didn’t really think I’d ever be going back to read old dengue literature but these days my prior gained knowledge on certain antibody mechanisms that is well characterized in dengue is important in thinking about SARS-CoV-2. And, assays we will be using to test vaccine responses from the trial were rapidly developed using knowledge from my dengue work.
6. In a recent publication you demonstrated that, despite SARS Cov-S and 2019-nCoV S having similar structural homology, there was no cross reactivity with three potent SARS-CoV RBD monoclonal antibodies. How does that finding affect how you proceed?
It doesn’t. We are specifically using SARS-CoV-2 spike here that will elicit specific antibodies.
7. In your research, you pioneered a technique to effectively stabilise coronavirus ‘s’ spikes as they can transition from one conformational state to another. Could you briefly explain how this technique works and how it is beneficial to the development of vaccines?
Fusion is a function of viral proteins that facilitated the viral and host cell membranes to fuse and then infection ensues. There is a prefusion form of these proteins and a postfusion form. The best immune responses target the prefusion form thus we are using a prefusion spike in our vaccine, inclusive of the mutations you read about for other coronavirus spike proteins.
8. In 2019, you published a paper detailing how you designed nanoparticles that can target more conserved target sites of the Influenza A virus. Is the ultimate goal to create more broad-spectrum vaccines? How viable could that be for coronaviruses?
Yes, that is in fact the idea for that flu vaccine. We call that a “universal influenza vaccine strategy”. It is definitely a viable strategy for coronaviruses and other large viral families that share genetic similarities.
9. What advice would you give to other women aspiring to pursue a career in science?
1. Come to slay, everyday. 2. Speak up confidently. 3. Demand a seat at the table… at the head of the table.
And, seriously find a set of mentors who believe in diversity and inclusion and who are willing to fight for your voice to be heard and your seat to remain. That’s exactly who Dr. Barney Graham, my boss, has been to me.




